MedAustron offers a highly precise and innovative form of radiation therapy with protons and carbon ions, the so-called ion beam or particle therapy. Compared to conventional radiotherapy with photons, particle therapy is able to reduce the radiation exposure of the adjacent healthy tissue and almost completely spare the tissue behind the tumor. Therefore, particle therapy is an ideal treatment for tumors close to radiation-sensitive organs, such as the brain, spinal cord, eyes or lungs. Since strongly growing tissue reacts more sensitively to radiation, proton therapy is particularly suitable for cancer in children and adolescents. By minimizing the dose delivered to healthy tissue, the risk of long-term side effects such as hormone and growth disorders or secondary malignancies can be reduced. In terms of treatment efficiency, particle therapy offers higher biological effectiveness compared to conventional radiotherapy. This is especially true for the treatment of radiation-resistant tumors, such as sarcomas or melanomas.
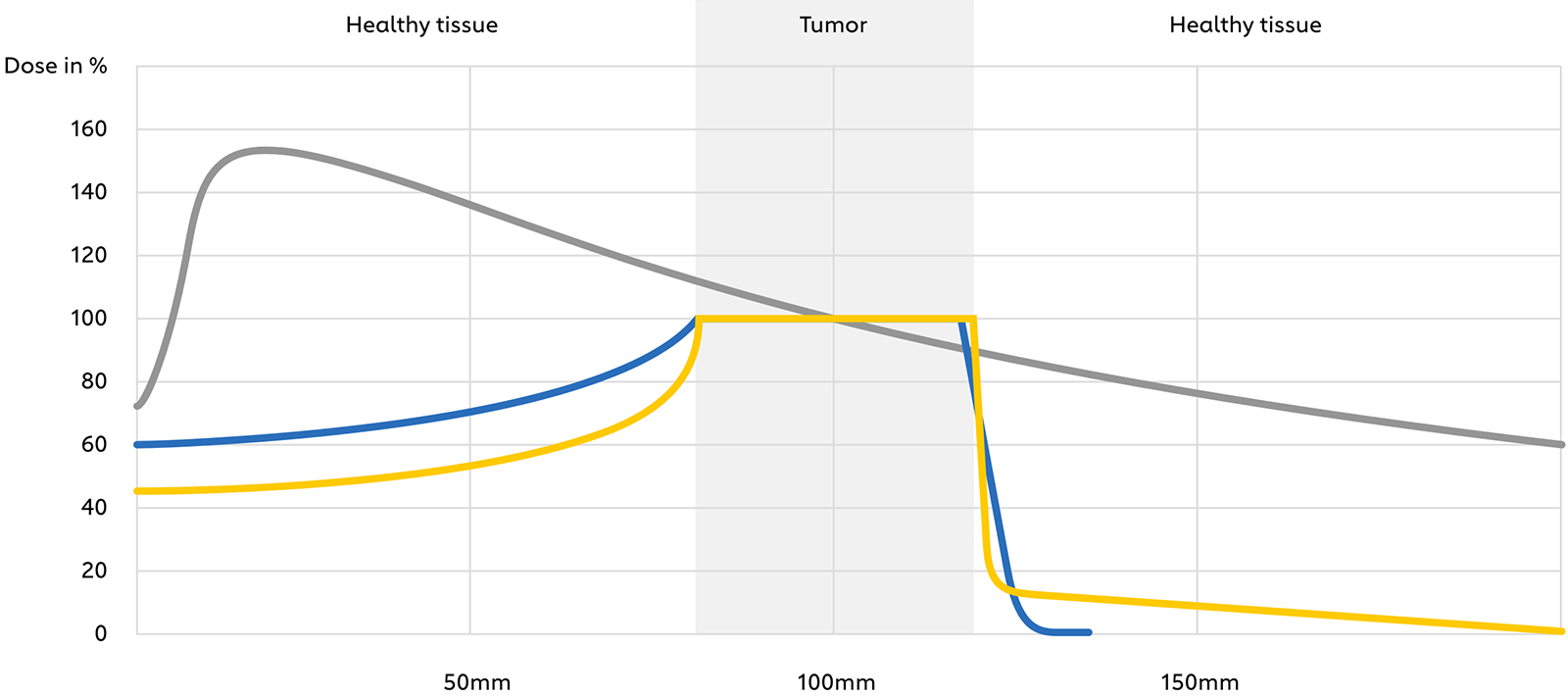
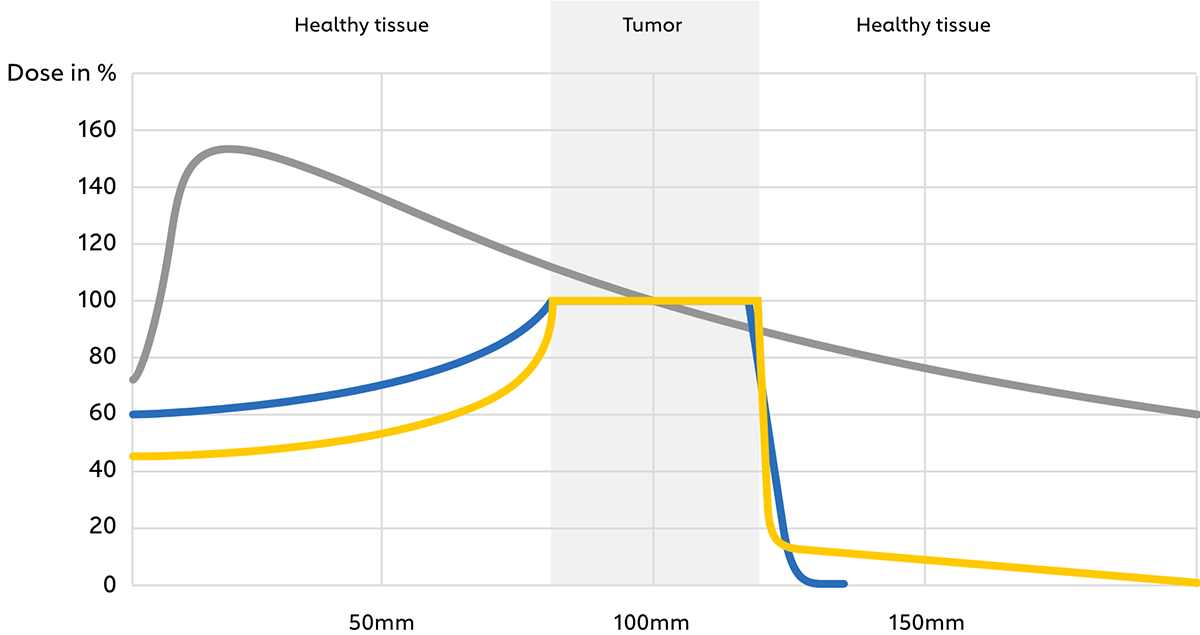
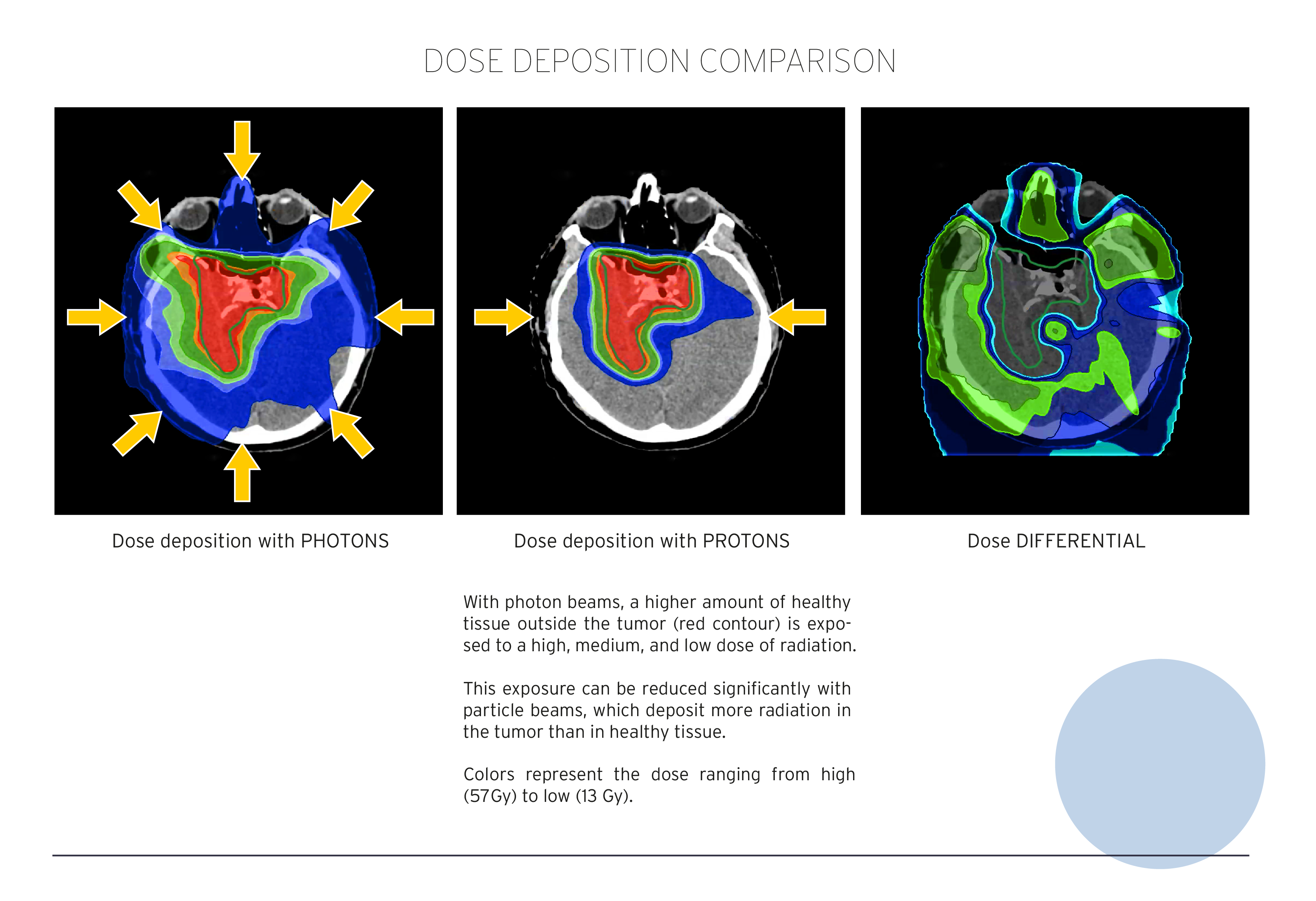
Fig. 1: Depth-dose profile of photons (conventional radiotherapy) as well as protons and carbon ions (particle therapy) in tissue.
Special features of particle or ion beam therapy
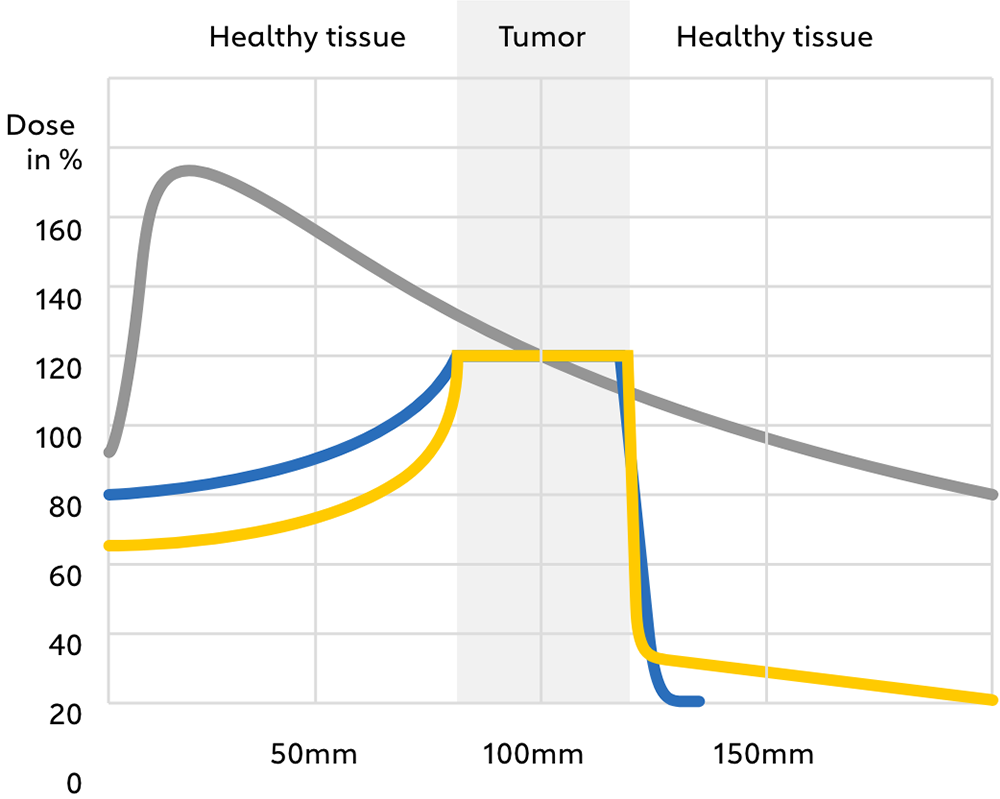
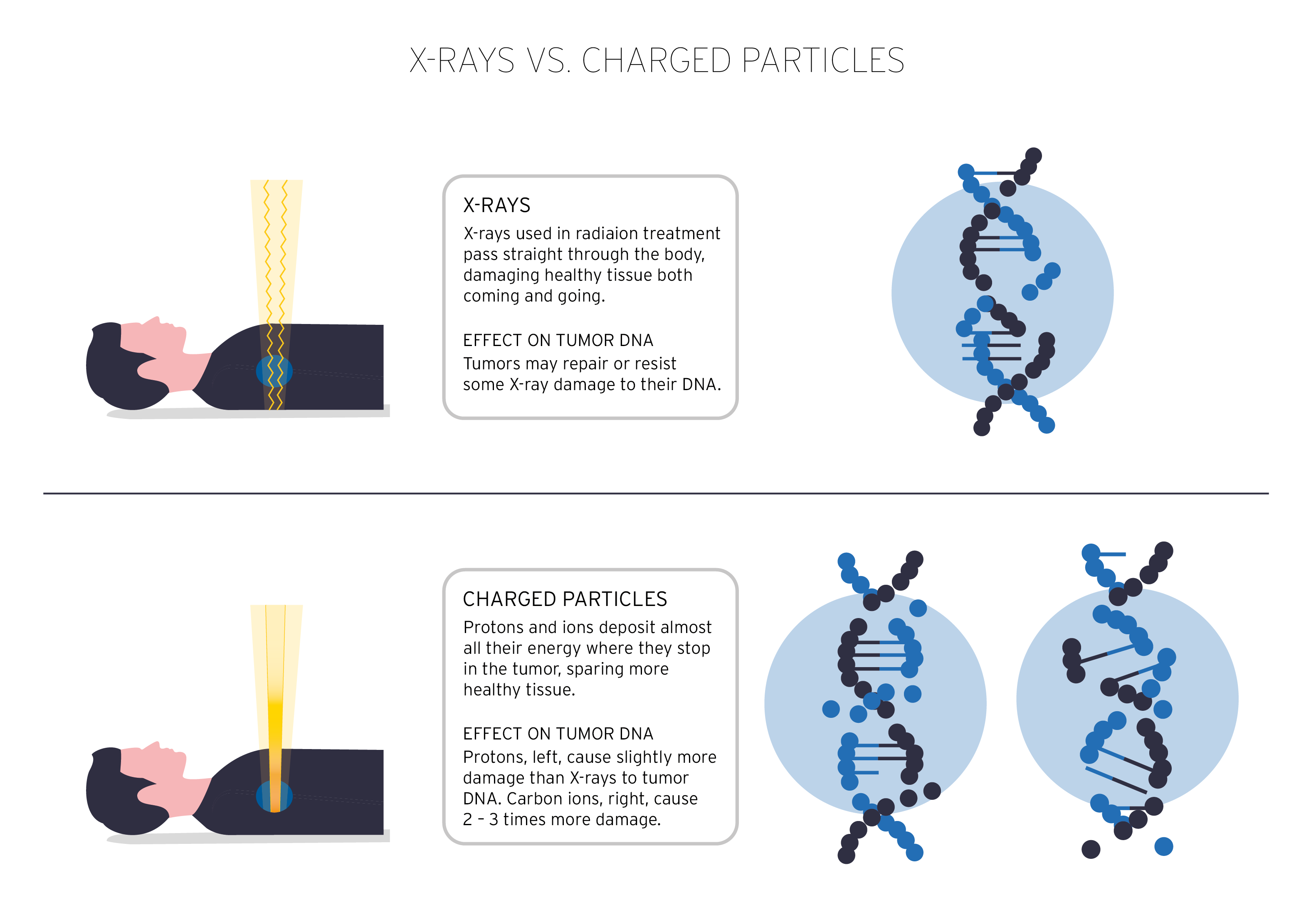
Compared to photons (e.g. gamma rays, X-rays), which are electromagnetic fields from a physical point of view, protons and carbon ions are charged, massive particles. These properties result in several biophysical advantages when passing through mass: a lower input dose proximal to the tumor, an almost complete energy deposition at the tumor site (corresponding to a so-called “Bragg peak”, see Fig. 1), and almost no output dose deposition in the tissue distal to the tumor (Figs. 2,3). This results in a reduced dose to nearby healthy organs and thus less toxicity, as well as safer delivery of a higher radiation dose to the tumor, especially if it is located close to critical organs. All in all, these effects may improve both the therapeutic relationship due to reduced toxicity and local tumor control and survival.
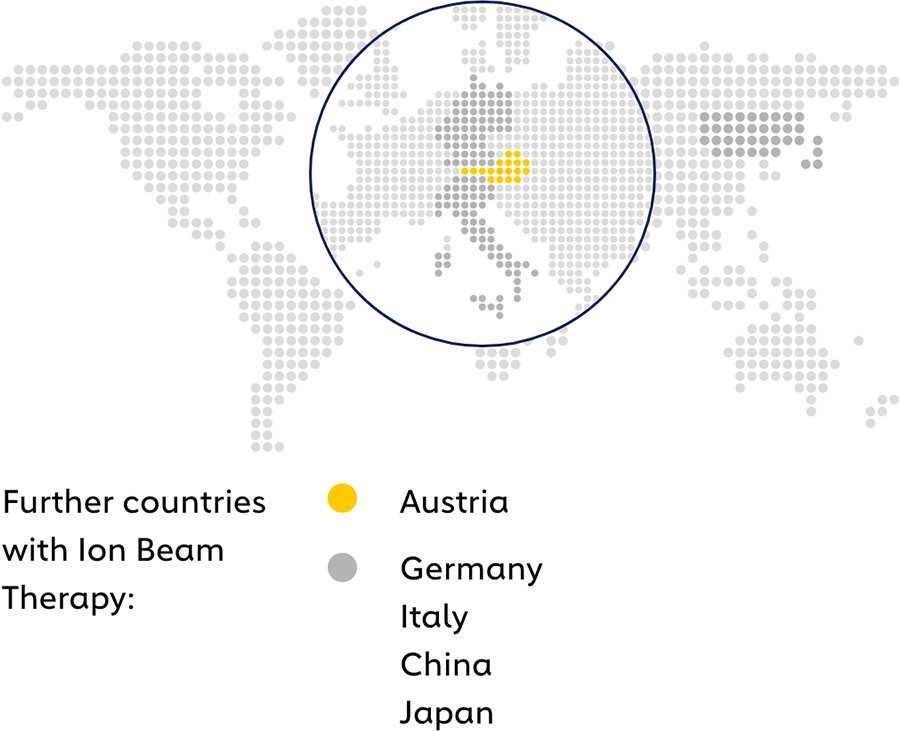
Centers with proton AND carbon ion therapy
Austria
Special features of therapy with carbon ions
The effectiveness of radiotherapy in killing tumor cells is determined by the type of radiation. Their quality is measured by the linear energy transfer LET, which indicates the ionization density of the mass passed through by radiation. Compared to photons inducing weak ionization of mass (low-LET irradiation), carbon ions produce high-density ionization events per length unit (high-LET irradiation), which are responsible for very complex tumor cell injuries (Fig. 3). Typically, low-LET irradiation induces predominantly repairable DNA damage leading to tumor cell survival, while high-LET irradiation causes highly complex, non-repairable DNA damage leading to cell death. This effective, non-repairable DNA damage is about 20% after low-LET irradiation and about 70% after high-LET irradiation. The relative biological effectiveness (RBE) of particles is therefore higher than that of photons.
This means that protons and carbon ions kill more tumor cells than photons at the same radiation dose. This is especially true for carbon ions, whose RBE is 3-4 times higher compared to photons. This makes carbon ion therapy particularly suitable for tumors that are traditionally resistant to conventional radiotherapy, such as bone and soft tissue sarcomas, slow-growing tumors, local recurrences after conventional radiotherapy, or hypoxic (oxygen-deficient) tumors that are particularly resistant to radiation. Several studies, both preclinical and clinical, have shown that such tumors that are resistant to conventional radiotherapy can often be successfully treated with carbon ions. These facts help to add a new, optimistic dimension to the fight against cancer.
Schematic diagram of irradiation and effectiveness of ion beam therapy
Advantage in a nutshell
Ion beam or particle therapy reduces the risk of side effects and long-term side effects:
Particle therapy can not only increase the chances of healing cancer that is difficult to treat, but also improves the patient’s quality of life at the same time.
Please contact us
Do you have any questions about ion beam therapy or MedAustron?
Do you have any questions about the therapy or procedure? Whatever you want to know, do not hesitate to contact us. We will get back to you within two business days.
Contact Therapy request